Signed in as:
filler@godaddy.com
Signed in as:
filler@godaddy.com
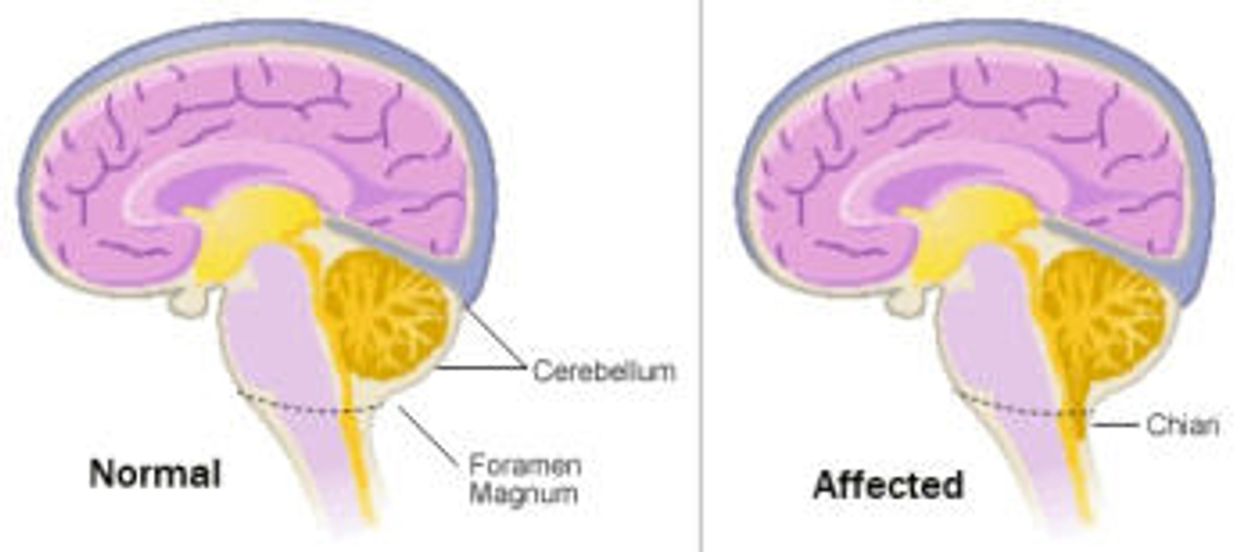
Chiari Malformations (CM)(key-Ar-ee—mal-for-May-Shun) are structural defects in the cerebellum, the part of the brain that controls balance. Normally the cerebellum and parts of the brain stem sit in an indented space at the lower rear of the skull, above the foramen magnum (a funnel-like opening to the spinal canal). When part of the cerebellum is located below the foramen magnum, it is called a Chiari malformation. CM may develop when the bony space is smaller than normal, causing the cerebellum and brain stem to be pushed downward into the foramen magnum and into the upper spinal canal. The resulting pressure on the cerebellum and brain stem may affect functions controlled by these areas and block the flow of cerebrospinal fluid (CSF)— the clear liquid that surrounds and cushions the brain and spinal cord—to and from the brain.
What causes these malformations?
CM has several different causes. It can be caused by structural defects in the brain and spinal cord that occur during fetal development, whether caused by genetic mutations or lack of proper vitamins or nutrients in the maternal diet. This is called primary or congenital CM. It can also be caused later in life if spinal fluid is drained excessively from the lumbar or thoracic areas of the spine either due to injury, exposure to harmful substances, or infection. This is called acquired or secondary CM. Primary CM is much more common than secondary CM.
How are they classified?
CM are classified by the severity of the disorder and the parts of the brain that protrude into the spinal canal.Type I involves the extension of the cerebellar tonsils (the lower part of the cerebellum) into the foramen magnum, without involving the brain stem.Normally, only the spinal cord passes through this opening. Type I—which may not cause symptoms—is the most common form of CM and is usually first noticed in adolescence or adulthood, often by accident during an examination for another condition. Type I is the only type of CM that can be acquired. Type II, also called classic CM, involves the extension of both cerebellar and brain stem tissue into the foramen magnum. Also, the cerebellar vermis (the nerve tissue that connects the two halves of the cerebellum) may be only partially complete or absent. Type II is usually accompanied by a myelomeningocele—a form of spina bifida that occurs when the spinal canal and backbone do not close before birth, causing the spinal cord and its protective membrane to protrude through a sac-like opening in the back. A myelomeningocele usually results in partial or complete paralysis of the area below the spinal opening. The term Arnold-Chiari malformation (named after two pioneering researchers) is specific to Type II malformations. Type III is the most serious form of CM. The cerebellum and brain stem protrude, or herniate, through the foramen magnum and into the spinal cord.Part of the brain’s fourth ventricle, a cavity that connects with the upper parts of the brain and circulates CSF, may also protrude through the hole and into the spinal cord. In rare instances, the herniated cerebellar tissue can enter an occipital encephalocele, a pouch-like structure that protrudes out of the back of the head or the neck and contains brain matter. The covering of the brain or spinal cord can also protrude through an abnormal opening in the back or skull. Type III causes severe neurological defects. Type IV involves an incomplete or underdeveloped cerebellum—a condition known as cerebellar hypoplasia. In this rare form of CM, the cerebellar tonsils are located in a normal position but parts of the cerebellum are missing, and portions of the skull and spinal cord may be visible. Another form of the disorder, under debate by some scientists, is Type 0, in which there is no protrusion of the cerebellum through the foramen magnum but headache and other symptoms of CM are present.
What are the symptoms of a Chiari malformation?
Individuals with CM may complain of neck pain, balance problems, muscle weakness, numbness or other abnormal feelings in the arms or legs, dizziness, vision problems, difficulty swallowing, ringing or buzzing in the ears, hearing loss, vomiting, insomnia, depression, or headache made worse by coughing or straining. Hand coordination and fine motor skills may be affected. Symptoms may change for some individuals, depending on the build-up of CSF and resulting pressure on the tissues and nerves. Persons with a Type I CM may not have symptoms. Adolescents and adults who have CM but no symptoms initially may, later in life, develop signs of the disorder. Infants may have symptoms from any type of CM and may have difficulty swallowing, irritability when being fed, excessive drooling, a weak cry, gagging or vomiting, arm weakness, a stiff neck, breathing problems, developmental delays, an inability to gain weight, and more. Because our bodies are different, symptoms may vary from patient to patient.
How common are Chiari malformations?
In the past, it was estimated that the condition occurs in about one in every 1,000 births. However, the increased use of diagnostic imaging has shown that CM may be much more common. Complicating this estimation is the fact that some children who are born with the condition may not show symptoms until adolescence or adulthood, if at all. CM occur more often in women than in men and Type II malformations are more prevalent in certain groups, including people of Celtic descent.
Are other conditions associated with Chiari malformations?
Individuals who have a CM often have these related conditions:Hydrocephalus is an excessive build-up of CSF in the brain. A CM can block the normal flow of this fluid, resulting in pressure within the head that can cause mental defects and/or an enlarged or misshapen skull. Severe hydrocephalus, if left untreated, can be fatal. The disorder can occur with any type of CM, but is most commonly associated with Type II. Spina bifida is the incomplete development of the spinal cord and/or its protective covering. The bones around the spinal cord don’t form properly, leaving part of the cord exposed and resulting in partial or complete paralysis. Individuals with Type II CM usually have a myelomeningocele, a form of spina bifida in which the bones in the back and lower spine don’t form properly and extend out of the back in a sac-like opening. Syringomyelia, or hydromyelia, is a disorder in which a CSF-filled tubular cyst, or syrinx, forms within the spinal cord’s central canal. The growing syrinx destroys the centre of the spinal cord, resulting in pain, weakness, and stiffness in the back, shoulders, arms, or legs. Other symptoms may include headaches and a loss of the ability to feel extremes of hot or cold, especially in the hands. Some individuals also have severe arm and neck pain. Tethered cord syndrome occurs when the spinal cord attaches itself to the bony spine. This progressive disorder causes abnormal stretching of the spinal cord and can result in permanent damage to the muscles and nerves in the lower body and legs. Children who have a myelomeningocele have an increased risk of developing a tethered cord later in life. Spinal curvature is common among individuals with Syringomyelia or CM Type I. Two types of spinal curvature can occur in conjunction with CM:scoliosis, a bending of the spine to the left or right; and kyphosis, a forward bending of the spine. Spinal curvature is seen most often in children with CM, whose skeleton has not fully matured. CM may also be associated with certain hereditary syndromes that affect neurological and skeletal abnormalities, other disorders that affect bone formation and growth, fusion of segments of the bones in the neck, and extra folds in the brain.
How are Chiari malformations diagnosed?
Many people with CM are misdiagnosed and their malformations are discovered only during the course of diagnosis or treatment for another disorder. The doctor will perform a physical exam and check the person’s memory, cognition, balance (a function controlled by the cerebellum), touch, reflexes, sensation, and motor skills (functions controlled by the spinal cord). The physician may also order one of the following diagnostic tests: An X-ray uses electromagnetic energy to produce images of bones and certain tissues on film. An X-ray of the head and neck cannot reveal a CM but can identify bone abnormalities that are often associated with CM. This safe and painless procedure can be done in a doctor’s office and takes only a few minutes. Computed tomography (also called a CT scan) uses X-rays and a computer to produce two-dimensional pictures of bone and vascular irregularities, certain brain tumors and cysts, brain damage from head injury, and other disorders. Scanning takes about 3 to 5 minutes. This painless, noninvasive procedure is done at an imaging center or hospital on an outpatient basis and can identify hydrocephalus and bone abnormalities associated with CM. Magnetic resonance imaging (MRI) is the imaging procedure most often used to diagnose a CM. Like CT, it is painless and non-invasive and is performed at an imaging center or hospital. MRI uses radio waves and a powerful magnetic field to produce either a detailed three-dimensional picture or a two-dimensional “slice” of body structures, including tissues, organs, bones, and nerves. Depending on the part(s) of the body to be scanned, MRI can take up to an hour to complete. MRI is the most reliable method of diagnosing CM.

How are they treated?
Some CM are asymptomatic. In other cases, medications may manage certain symptoms, such as pain. Surgery is the only treatment available to correct functional disturbances or halt the progression of damage to the central nervous system. Most individuals who have surgery see a reduction in their symptoms and/or prolonged periods of relative stability. More than one surgery may be needed to treat the condition. Posterior fossa decompression surgery is performed on adults with CM to create more space for the cerebellum and to relieve pressure on the spinal column. Surgery involves making an incision at the back of the head and removing a small portion of the bottom of the skull (and sometimes part of the spinal column) to correct the irregular bony structure. The neurosurgeon may use a procedure called electrocautery to shrink the cerebellar tonsils.This surgical technique involves destroying tissue with high-frequency electrical currents. A related procedure, called a spinal laminectomy, involves the surgical removal of part of the arched, bony roof of the spinal canal (the lamina) to increase the size of the spinal canal and relieve pressure on the spinal cord and nerve roots. The surgeon may also make an incision in the dura (the covering of thebrain) to examine the brain and spinal cord. Additional tissue may be added to the dura to create more space for the flow of CSF. Infants and children with myelomeningocele may require surgery to reposition the spinal cord and close the opening in the back. Hydrocephalus may be treated with a shunt system that drains excess fluid and relieves pressure inside the head. A sturdy tube that is surgically inserted into the head is connected to a flexible tube that is placed under the skin, where it can drain the excess fluid into either the chest wall or the abdomen so it can be absorbed by the body. An alternative surgical treatment to relieve hydrocephalus is third ventriculostomy, a procedure that improves the flow of CSF. A small perforation is made in the floor of the third ventricle and the CSF is diverted into the subarachnoid space to relieve pressure. Similarly, surgeons may open the spinal cord and insert a shunt to drain a syringomyelia or hydromyelia. A small tube or catheter may be inserted into the syrinx for continued drainage.
What research is being done?
Within the Federal government, the National Institute of Neurological Disorders and Stroke (NINDS), a component of the National Institutes of Health (NIH), supports and conducts research on brain and nervous system disorders, including Chiari malformations. The NINDS conducts research in its laboratories at the NIH, in Bethesda, Maryland, and supports research through grants to major medical research institutions across the country. In one study, NINDS scientists are trying to better understand the genetic factors responsible for the malformation by examining individuals with CM who have a family member with either a CM or syringomyelia. NINDS scientists are examining individuals who either have Syringomyelia or are at risk of developing the disorder, including patients with Chiari I malformation. By recording more than 5 years of symptoms, muscle strength, general level of functioning, and MRI scan findings from individuals who receive standard treatment for Syringomyelia, researchers can obtain more information about factors that influence its development, progression, and relief of symptoms. Study results may allow scientists to provide more accurate recommendations to future patients with syringomyelia regarding optimal surgical or non-surgical treatment of their condition. AN NIH study is reviewing an alternative surgical treatment for syringomyelia. By examining people with syringomyelia, in which there is an obstruction in CSF flow, NIH scientists hope to learn whether a surgical procedure that relieves the obstruction in CSF flow can correct the problem without having to cut into the spinal cord itself. The NIH’s Management of Myelomeningocele Study is comparing prenatal surgery to the conventional post-birth approach of closing the opening in the spine and back that is common to some forms of CM. The study will enroll 200 women whose fetuses have spina bifida and will compare the safety and efficacy of the different surgeries. Preliminary clinical evidence of intrauterine closure of the myelomeningocele suggests the procedure reduces the incidence of shunt dependent hydrocephalus and restores the cerebellum and brain stem to more normal configuration. At 1 year and 2 ½ years after surgery the children will be tested for motor function, developmental progress, and bladder, kidney, and brain development.

Chiari Malformations (CM)(key-Ar-ee—mal-for-May-Shun) are structural defects in the cerebellum, the part of the brain that controls balance. Normally the cerebellum and parts of the brain stem sit in an indented space at the lower rear of the skull, above the foramen magnum (a funnel-like opening to the spinal canal). When part of the cerebellum is located below the foramen magnum, it is called a Chiari malformation.

Syringomyelia (sear-IN-go-my-EEL-ya) is a disorder in which a cyst forms within the spinal cord. This cyst, called a syrinx, expands and elongates over time, destroying a portion of the spinal cord from its centre and expanding outward. As a syrinx widens it compresses and injures nerve fibres that carry information from the brain to the extremities.

Chronic diseases such as diabetes, cancer, arthritis, mental illness, and cardiovascular and chronic respiratory diseases are major contributors to reduced quality of life, loss of productivity, and increased hospitalization and health care costs as well as premature death in Canada. Out of every 5 Canadians aged 20 years or older, 3 have a chronic disease and 4 are at risk of developing a chronic condition.

Chronic diseases such as diabetes, cancer, arthritis, mental illness, and cardiovascular and chronic respiratory diseases are major contributors to reduced quality of life, loss of productivity, and increased hospitalization and health care costs as well as premature death in Canada. Out of every 5 Canadians aged 20 years or older, 3 have a chronic disease and 4 are at risk of developing a chronic condition.
REGISTERED CHARITY #: 802775791RR0001
TOGETHER WE ARE STRONGER®
www.carionfenn.org - smcm@carionfenn.org
A place to share, learn and support each other.
Copyright © 2015 - 2026 Carion Fenn Foundation - All Rights Reserved.
Policies, Media Disclaimer & Consent Policy
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.